An ectopic pregnancy is one that grows outside the uterus (womb) , 1 in 90 pregnancies (just over 1%) is an ectopic pregnancy. Women who have had a previous ectopic pregnancy are at higher risk. A pregnancy cannot survive in these situations and it can pose a serious risk to you.
In a normal pregnancy, the fertilised egg moves from the fallopian tube into the uterus, where the pregnancy grows and develops. If this does not happen, the fertilised egg may implant and start to develop outside the uterus, leading to an ectopic pregnancy.
An ectopic pregnancy can be life-threatening because as the pregnancy advances it can burst (rupture), causing severe pain and internal bleeding.

From Ovulation to implantation
Most ectopic pregnancies develop in the fallopian tubes (tubal pregnancy) but, rarely (3–5 out of 100 ectopic pregnancies), can occur in other places.

Sites for Ectopic pregnancy
Each woman is affected differently by an ectopic pregnancy. Some women have no symptoms, some have a few symptoms, while others have many symptoms. Most women get physical symptoms in the 6th week of pregnancy (about 2 weeks after a missed period). You may or may not be aware that you are pregnant if your periods are irregular, or if the contraception you are using has failed.
Because symptoms vary so much, it is not always straight forward to reach a diagnosis of an ectopic pregnancy.
The symptoms of an ectopic pregnancy may include:
Pain in your lower abdomen: This may develop suddenly for no apparent reason or may come on gradually over several days. It may be on one side only.
Vaginal bleeding: You may have some spotting or bleeding that is different from your normal period. The bleeding may be lighter or heavier or darker than normal.
Pain in the tip of your shoulder: This pain is caused by blood leaking into the abdomen and is a sign that the condition is getting worse. This pain is there all the time and may be worse when you are lying down. It is not helped by movement and may not be relieved by painkillers. You should seek urgent medical advice if you experience this.
Upset tummy: You may have diarrhoea, or feel pain on opening your bowels.
Severe abdominal pain/collapse: If the fallopian tube bursts (ruptures) and causes internal bleeding, you may develop intense abdominal pain or you may collapse.
In rare instances, collapse may be the very first sign of an ectopic pregnancy. This is an emergency situation and you should seek urgent medical attention.
Most ectopic pregnancies are suspected between 6 and 10 weeks of pregnancy. Sometimes the diagnosis is made quickly. However, if you are in the early stages of pregnancy, it can take longer (a week or more) to make a diagnosis of an ectopic pregnancy.
Your diagnosis will be made based on the following:
Treatment options may include medical treatment with methotrexate or surgical operation.
Because an ectopic pregnancy cannot lead to the birth of a baby, all options will end the pregnancy in order to reduce the risks to your own health.
Your options depend upon:
The treatment options for tubal ectopic pregnancy are listed below –
In certain circumstances, an ectopic pregnancy may be treated by medication (drugs). The fallopian tube is not removed. A drug (methotrexate) is given as an injection – this prevents the ectopic pregnancy from growing and the ectopic pregnancy gradually disappears.
Most women only need one injection of methotrexate for treatment. However, 15 in 100 women (15%) need to have a second injection of methotrexate.
If your pregnancy is beyond the very early stages or the βhCG level is high, methotrexate is less likely to succeed. Seven in 100 women (7%) will need surgery even after medical treatment.
In a case of failure of medical treatment you may need to undergo surgical treatment.
You will be asked to return sooner if you have any symptoms.
If you have opted for medical treatment, it is advisable that you should be under monitoring of your doctor because in some cases you may have to undergo for surgery in an emergency situation.
Surgical treatment
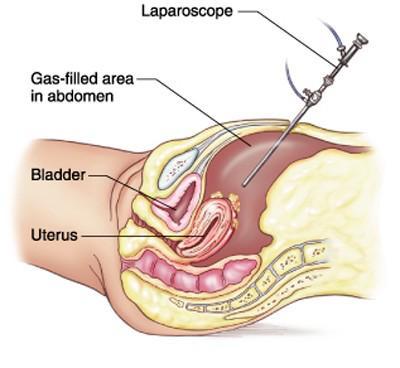
An operation to remove the ectopic pregnancy is another option.
The surgery will either be:
Laparoscopy (known as keyhole surgery): Your stay in hospital is shorter (24–36 hours)and physical recovery is quicker than after open surgery.
Open surgery (known as a laparotomy): This is done through a larger cut in your abdomen and may be needed if severe internal bleeding is suspected. You will need to stay in hospital for2–4 days. It usually takes about 4–6 weeks to recover. Options are salpingectomy/salpingotomy
To reduce the risk of having another ectopic pregnancy, you will usually be advised to have your affected fallopian tube removed, (this is known as salpingectomy).
Salpingotomy - aims to remove the pregnancy without removing the tube. It carries a higher risk of a future ectopic pregnancy. Some women may need further medical treatment or another operation to remove the tube later if the pregnancy has not been completely removed during salpingotomy.
The decision to perform salpingectomy or salpingotomy may sometimes only be made during laparoscopy under anaesthesia.
This treatment modalities are available at our SAAVI women’s hospital.