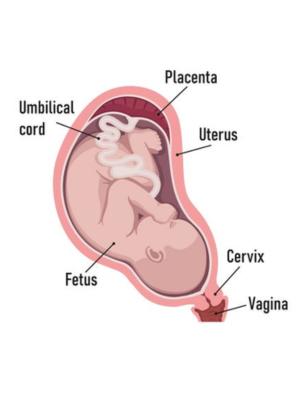
Normal Placenta
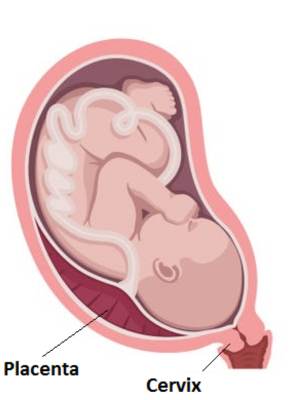
Low-lying Placenta (Less than 20mm from the cervix)

Placenta Praevia (Completely covering the cervix)
If your placenta is low lying at your 20-week scan, you will be offered a follow-up scan at 32 weeks of pregnancy to see whether it is still low lying. This may include a transvaginal scan. You should be offered a further ultrasound scan at 36 weeks if your placenta is still low lying.
If you have placenta praevia at 34-36 weeks , you are at higher risk of having your baby early (less than 37 weeks) and you may be offered a course of steroid injections between 34 and 36 weeks of pregnancy to help your baby to become more mature. ( Corticosteroids in pregnancy )
If you go into labour early, you may be offered a type of medication (known as tocolysis) that is given to try to stop your contractions and to allow you to receive a course of steroids.
Even if you have had no symptoms before, there is a small risk that you could bleed suddenly and heavily, which may mean that you need an emergency caesarean.
If you know you have a low-lying placenta, you should contact the hospital straight away if you have any vaginal bleeding, contractions or pain. If you have bleeding, your doctor may need to do a speculumexamination to check how much blood loss there is and where it is coming from. This is a safe examination.
You should try to avoid becoming anemic ( low hemoglobin ) during pregnancy by having a healthy diet by taking iron supplements oriron injection if recommended by your doctor. Your blood haemoglobin levels (a measure of whether you are anaemic) will be checked at regular intervals during your pregnancy bysimple test called CBC.
We at SAAVI women’s hospital recommend & will support you to maintain your Hb level @12gm% .
Our dietician will help in choosing right diet for you.
Your doctor will discuss with you the safest way for you to give birth based on your own individual circumstances.
If the edge of your placenta is less than 20 mm from the entrance to the cervix on your scan at 36 weeks, a caesarean will be the safest way for you to give birth. If the placenta is further than 20 mm from your cervix you can choose to have a vaginal birth.
Unless you have heavy or recurrent bleeding, your caesarean will usually take place between 36 and 37 weeks. If you have had vaginal bleeding during your pregnancy, your caesarean may need to take place earlier than this.
During your caesarean, you may have heavier than average bleeding. There are many different things that your doctors can do to stop the bleeding, but if it continues and cannot be controlled in other ways, a hysterectomy (removal of your uterus) may be needed.
If you have heavy bleeding before your planned date of delivery, you may be advised to have your baby earlier than expected.
If you have placenta praevia, you are more likely to need a blood transfusion, particularly if you have very heavy bleeding. During a planned caesarean, blood should be available for you if needed.
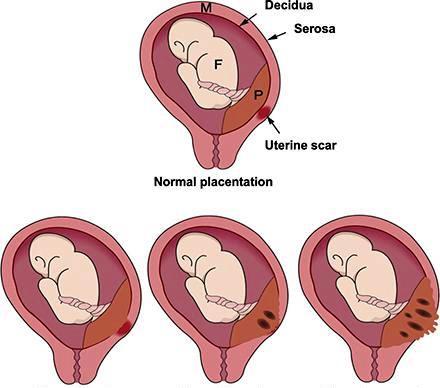
Placenta accrete spectrum
Placenta accreta spectrum, formerly known as morbidly adherent placenta, refers to the range of pathologic adherence of the placenta to muscle of uterus,
Types of placental problems will depend upon myometrial invasion of placenta.
Placenta accreta is less severe form of myometrial invasion.
Placenta increta and percreta is the more severe form of invasion.
Placenta accrete spectrum is a rare (between 1 in 1000 and 1 in 2000) complication of pregnancy. This is when the placenta grows into the muscle of the uterus, making delivery of the placenta at the time of birth very difficult.
Placenta accreta is more common in women with placenta praevia who have previously had one or more caesarean births, but it can also occur if you have had other surgery to your uterus, or if you have a uterine abnormality such as fibroids or a bicornuate uterus.
Placenta accreta may be suspected during the ultrasound scans that you will have in your pregnancy. Additional tests such as magnetic resonance imaging (MRI) scans may help with the diagnosis.
If placenta accreta is suspected before your baby is born, Your doctor will advise for removal of uterus with intact placenta, after delivery of a baby
There may be bleeding when an attempt is made to deliver your placenta after your baby has been born. The bleeding can be heavy and you may require blood transfusion. There is a risk of injury to your bladder during this surgery.
Your doctor at SAAVI women’s hospital would discuss with you the option of a planned caesarean hysterectomy (removal of your uterus with the placenta still in place, straight after your baby is born) if placenta accreta is confirmed at sonography.
Placenta praevia happens when your placenta (afterbirth) attaches in the lower part of your uterus (womb), sometimes completely covering the cervix. This can cause heavy bleeding during pregnancy or at the time of birth. If you have placenta praevia, your baby will probably need to be born by caesarean.
Placenta accreta is a rare but serious condition when the placenta is stuck to the muscle of your womb and/or to nearby structures such as your bladder. This is more common if you have previously had a caesarean. It may cause heavy bleeding at the time of birth.