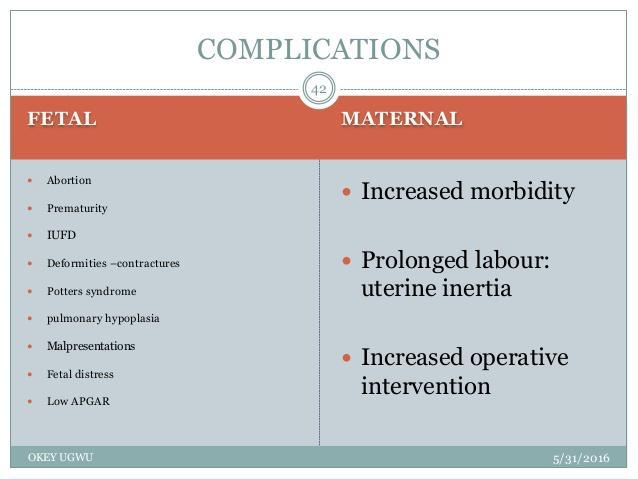
complications
function of Amniotic Sac

Premature Rupture Of Membranes
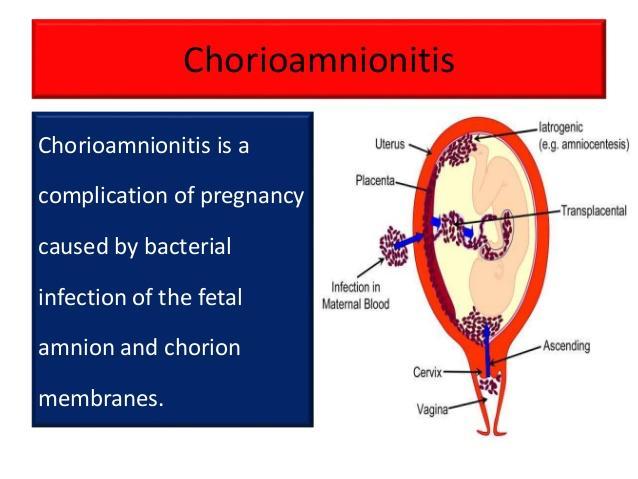
chorioamnionitis

Things to remember when your water broke
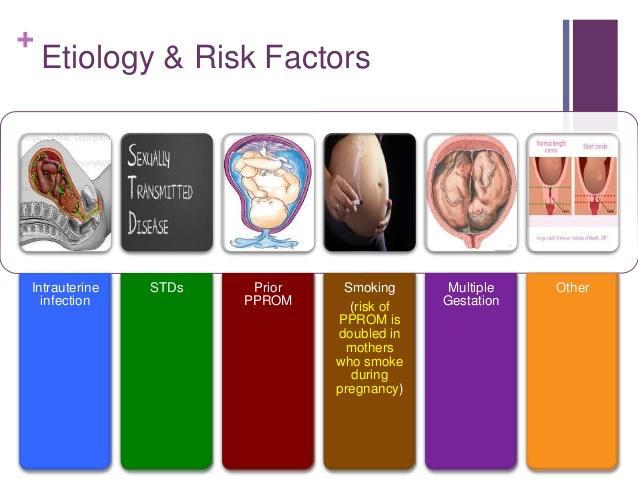
Etiology & Risk Factors

PMS & It's Effects
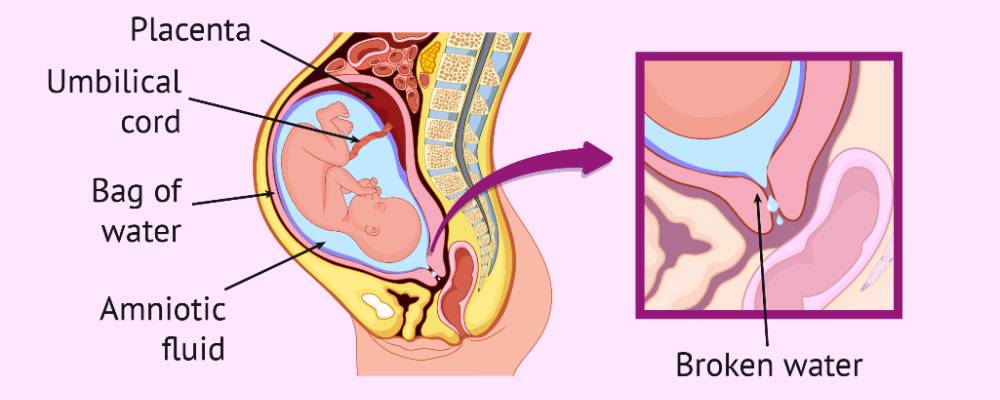
Preterm Prelabour Rupture of Membranes
PROM / PPROM is best diagnosed by a vaginal examination. your doctor will use a sterile speculum (an instrument used to separate the walls of the vagina) to look at your cervix and see whether the leaking fluid is amniotic fluid.
An ultrasound scan to estimate the amount of fluid around your baby is sometimes helpful.
If you and your baby are both well with no signs of infection or other problem then you may be advised to wait until 37 weeks to give birth. This is because carrying on with the pregnancy reduces the risk to your baby that are related to being born preterm.
Your doctor should discuss the timing of birth with you depending on your individual circumstances and preferences.