- Insertion of a cervical stitch takes place in an operating theatre. You may be given a general anesthetic, thanks to which, you will be asleep.
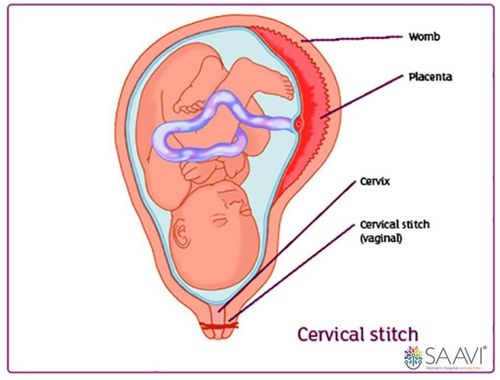
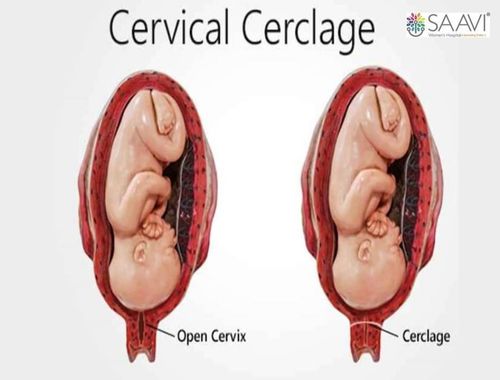
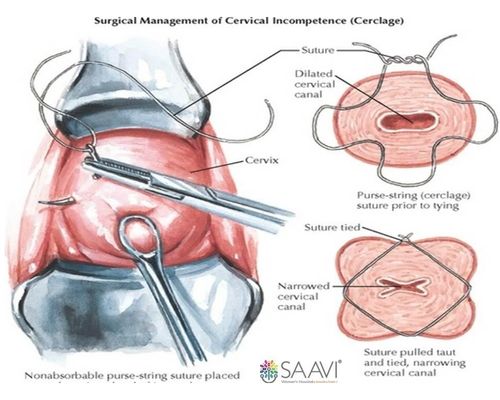
- In the operating theatre, your legs will be put in supports and sterile covers will be used to keep the operating area clean. The surgeon will hold the cervix and put a stitch around it (see the illustration). The stitch is then tightened and tied, helping to keep the cervix closed. The operation is called a transvaginal cerclage/os wiring/nylon wiring.
- You will be offered medication to ease any discomfort after the surgery. You will likely be able to go home the same day although you may be advised to stay in the hospital longer (if required).
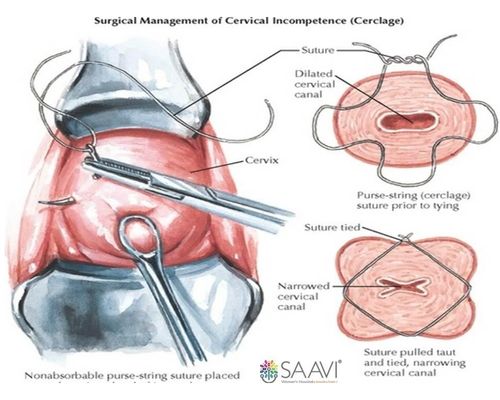
The transvaginal cervical stitch procedure (left) and once it is completed (right)